 |
| Large Intestine |
Features
The large intestine extends from the ileocaecal junction to the anus. It is about blind 1.5 m long, and is divided into the caecum (Latin blind pouch), the ascending colon, right colic flexure, the transverse colon, left colic flexure, the descending colon, the sigmoid colon, the rectum and the anal canal. In the angle between the caecum and the terminal part of the ileum, there is a narrow diverticulum called the vermiform appendix (Latin attachment). The general structure of large intestine is considered first followed by its parts one by one. The structure of the large intestine is adapted for storage of matter reaching it from the small intestines, and for absorption of fluid and solutes from it. The epithelium is absorptive (columnar), but villi are absent. Adequate lubrication for passage of its contents is provided by numerous goblet cells scattered in the crypts as well as on the surface of the mucous membrane. The presence of numerous solitary lymphatic follicles provides protection against bacteria present in the lumen of the intestine.
Relevant Features
The relevant features of the large intestine are as follows:
1 The large intestine is wider in calibre than the smal intestine. The calibre is greatest at its commencement. and gradually diminishes towards the rectum where it is dilated to form the rectal ampulla just above the anal canal.
2 The greater part of the large intestine is fixed, except for the appendix, the transverse colon and the sigmoid colon.
3 The longitudinal muscle coat forms only a thin layer in this part of the gut. The greater part of it forms three ribbon-like bands, called the taeniae coli. Proximally the taeniae converge at the base of the appendix, and distally they spread out on the terminal part of the sigmoid colon to become continuous with the longitudinal muscle coat of the rectum. In the caecum, the ascending colon, the descending colon and sigmoid colon the positions of taeniae are anterior or taenia libera; posteromedial or taenia mesocolica and posterolateral or taenia omentalis but in the transverse colon the corresponding positions of taenia are inferior, posterior and superior. One taenia, taenia libera, is placed anteriorly in the caecum, ascending, descending and sigmoid colon, but is placed inferiorly in the transverse colon. Second taenia, taenia mesocolica is present on the posteromedial surface of caecum, ascending, descending and sigmoid colon, but is placed posteriorly on transverse colon at the site of attachment of the transverse mesocolon. Third taenia, taenia omentalis, is situated postero- laterally in caecum, ascending, descending and sigmoid colon, but is situated on the anterosuperior surface four of greater omentum meet the transverse colon. This change in position is due to twist in transverse colon.
4 Since the taeniae are shorter than the circular muscle coat, the colon is puckered and sacculated.
5 Small bags of peritoneum filled with fat, and calle the appendices epiploicne (Greek to flgat on) are scattered over the surface of the large intestine, except tor appendix, the caecum and the rectum. These are most numerous on the sides of the sigmoid colon and on the posterior surface of the transverse colon.
6 The blood supply to the colon is derived from c marginal artery of Drummond. It is formed by co branches of superior and inferior mesenteric arteries. Terminal branches from the marginal artery are distributed to the intestine as long and short vessels, vasa longa and vasa brevia. The long arteries divide into anterior and posterior branches close to the mesocolic taenia to pass between the serous and muscular coats and reach the amesocolic taeniae. They gradually pierce the muscular coat and reach the submucosa. The anastomosis between the two amesocolic taeniae is extremely poor. So longitudinal incisions should be made along this line.
Short branches arise either from the marginal artery or from the long branches, and the majority of them at once sink into the bowel wall at the mesocolic border. The short and long branches together thus provide the mesocolic region of the wall with abundant blood supply. It is only the amesocolic region which has scanty blood supply. Subserous coat of long branches is intimately related to appendices epiploicae, to which they contribute branches. During removal of these appendages care must be taken not to pull on them in order to avoid traction on the subjacent vessel. Bowel wall is weakened where it is pierced by the vessels and at the sites of attachment of appendices epiploicae. Mucosa may herniate in these situations causing diverticulosis, with associated dangers of diverticulitis, fibrosis and stricture.
7 Lymph from the large intestine passes through four sets of lymph nodes.
a. Epicolic lymph nodes, lying on the wall of the gut.
b. Paracolic nodes, on the medial side of the ascending and descending colon and near the mesocolic border of the transverse and sigmoid colon.
c. Intermediate nodes, on the main branches of the vessels.
d. Terminal nodes, on the superior and inferior mesenteric vessels. In carcinoma of the colon, the related paracolic and intermediate lymph nodes have to be removed. Their removal is possible only after the ligature of the main branch of the superior or inferior mesenteric artery along which the involved lymph nodes lie. It is necessary, therefore, to remove a large segment of the bowel than is actually required by the extent of the disease, in order to avoid gangrene as a result of interference with the blood supply. It is always wise to remove the whole portion of the bowel supplied by the ligated vessel.
8 The nerve supply of the large intestine, barring the lower half of the anal canal, is both sympathetic and parasympathetic. The midgut territory receives its sympathetic supply from the coeliac and superior mesenteric ganglia (T11 to L1), and its para- sympathetic supply from the vagus. Both types of nerves are distributed to the gut through the superior mesenteric plexus.
The hindgut territory receives its sympathetic supply from the lumbar sympathetic chain (L1, L2), and its parasympathetic supply from the pelvic splanchnic nerve (nervi erigentes), both via the superior hypogastric and inferior mesenteric plexuses. Some parasym- pathetic fibres reach the colon along the posterior abdominal wall. The ultimate distribution of nerves in the gut is similar to that in the wall of the small intestine. The parasympathetic nerves are motor to the large intestine and inhibitory to the internal anal sphincter. The sympathetic nerves are largely vasomotor, but also motor to the internal anal sphincter, and inhibitory to colon. Pain impulses from the gut up to the descending colon travel through the sympathetic nerves, and from the sigmoid colon and rectum through the pelvic splanchnic nerves.
Functions of Colon
The functions of the colon are as follows:
1 Lubrication of faeces by mucus.
2 Absorption of the water, salts and the other solutes.
3 Bacterial flora of colon synthesises vitamin B.
4 Mucoid secretion of colon is rich in antibodies of IgA group, which protect it from invasion by micro- organisms.
5 The microvilli (apical tufts) of some columnar cells serve a sensory function.
Caecum
 |
| Anterior view of ileocaecal region |
Features
Caecum is a large blind sac (Latin blind) forming the commencement of the large intestine. It is situated in the right iliac fossa, above the lateral half of inguinal ligament. It communicates superiorly with ascending colon, medially at the level of caecocolic junction with ileum, and posteromedially with the appendix.
Dimensions
It is 6 cm long and 7.5 cm broad. It is one of those organs of the body that have greater width than the length. The other examples are the prostate, pons and pituitary.
Relations
 |
| Relations of caecum |
Anterior: Coils of intestine and anterior abdominal wall.
Posterior
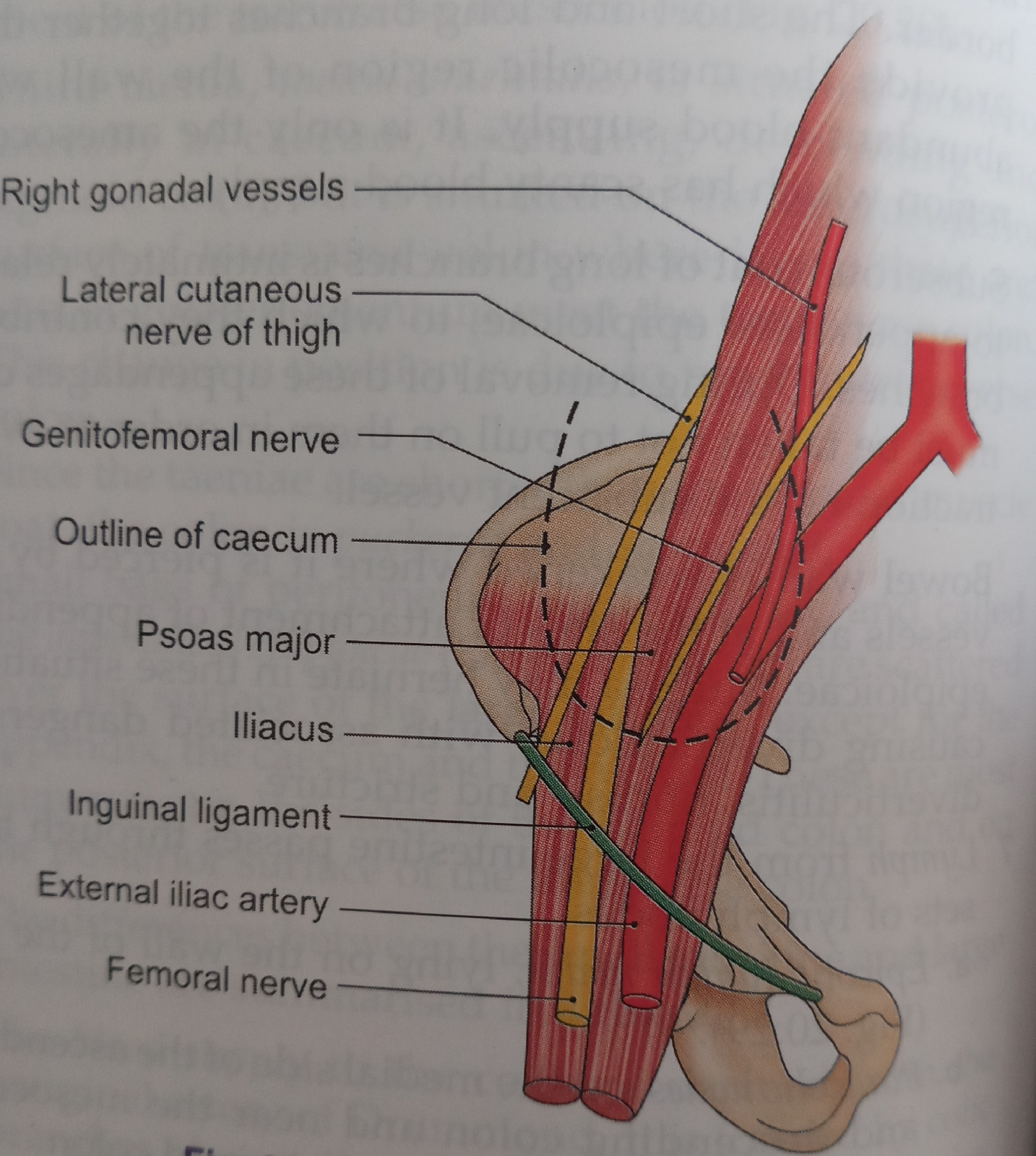
1 Muscles: Right psoas and iliacus
2 Nerves: Genitofemoral, femoral and lateral cutaneous nerve of thigh (all of the right side).
3 Vessels: Testicular or ovarian.
4 Appendix in the retrocaecal recess.
Vessels and Nerves
The arterial supply of the caecum is derived from the caecal branches of the ileocolic artery. The veins drain into the superior mesenteric vein. The nerve supply is same as that of the midgut (thoracic 11 to lumbar 1; parasympathetic, vagus).
DEVELOPMENT
 |
| Development of the caecum |
The caecum and appendix develop from the caecal bud arising from the postarterial segment of the midgut loop. The proximal part of the bud dilates to form the caecum. The distal part remains narrow to form the appendix. Thus initially the appendix arises from the apex of the caecum. However, due to rapid growth of the lateral wall of the caecum, the attachment of the appendix shifts medially.
ILEOCAECAL VALVE
 |
| The ileocaecal valve |
The lower end of the ileum opens on the posteromedial aspect of the caecocolic junction. The ileocaecal opening is guarded by the ileocaecal valve.
Structure
The valve has two lips and two frenula.
1 The upper lip is horizontal and lies at the ileocolic junction.
2 The lower lip is longer and concave, and lies at the ileocaecal junction.
The two frenula are formed by the fusion of the lips at the ends of the aperture. These are the left or anterior and the right or posterior frenula. The left end of the aperture is rounded, and the right end narrow and pointed.
Control and Mechanism
1 The valve is actively closed by sympathetic nerves, which cause tonic contraction of the ileocaecal sphincter.
2 It is mechanically closed by distension of the caecum.
Functions
1 It prevents reflux from caecum to ileum.
2 It regulates the passage of ileal contents into the caecum, and prevents them from passing too quickly.
Vermiform Appendix
 |
| Position oc appendix |
This is a worm-like diverticulum arising from the posteromedial wall, of the caecum, about 2 cm below the ileocaecal orifice.
Dimensions
The length varies from 2 to 20 cm with an average of 9 cm. It is longer in children than in adults. The diameter is about 5 mm. The lumen is quite narrow and may be obliterated after mid-adult life.
Positions
 |
| Position of the appendix according to the clock |
The appendix lies in the right iliac fossa. Although the base of the appendix is fixed, the tip can point in any direction, as described below. The positions are often compared to those of the hour hand of a clock.
1 The appendix may pass upwards and to the right. This is paracolic or 11 o'clock position.
2 It may lie behind the caecum or colon, known as retrocaecal or 12 o'clock position. This is the commonest position of appendix, about 65%.
3 The appendix may pass upwards and to the left. It points towards the spleen. This is the splenic or 2 o'clock position. The appendix may lie in front of the ileum (preileal) or behind the ileum (postileal). The preileal type is most dangerous type.
4 It may pass horizontally to the left (as if pointing to the sacral promontory called promontoric or 3 o'clock position.
5 It may descend into the pelvis called pelvic or 4 o'clock position. This is the second most common position about 30%.
6 It may lie below the caecum (subcaecal) and may point towards the inguinal ligament called as midinguinal or 6 o'clock position.
Appendicular Orifice
1 The appendicular orifice is situated on the postero- medial aspect of the caecum 2 cm below the ileocaecal orifice.
2 The appendicular orifice is occasionally guarded by an indistinct semilunar fold of the mucous membrane, known as the valve of Gerlach.
3 The orifice is marked on the surface by a point situated 2 cm below the junction of transtubercular and right lateral planes .
4 McBurney's point is the site of maximum tenderness in appendicitis. The point lies at the junction of lateral one-third and medial two-thirds of line joining the right anterior superior iliac spine to umbilicus.
Lumen of Appendix
It is quite small and may be partially or completely obliterated after mid-adult life.
Peritoneal Relations
The appendix is suspended by a small, triangular fold of peritoneum, called the mesoappendix, or appendicular mesentery. The fold passes upwards behind the ileum, and is attached to the left layer of the mesentery.
Blood Supply
 |
| Arterial supply of caecum and appendix |
The appendicular artery is a branch of the lower division of the ileocolic artery. It runs behind the terminal part of the ileum and enters the mesoappendix at a short distance from its base. Here it gives a recurrent branch which anastomoses with a branch of the posterior caecal artery. The main artery runs towards the tip of the appendix lying at first near to and then in the free border of the mesoappendix. The terminal part of the artery lies actually on the wall of the appendix.
Blood from the appendix is drained by the appendicular, ileocolic and superior mesenteric veins, to the portal vein.
Nerve Supply
Sympathetic nerves are derived from thoracic nine and ten segments through the coeliac plexus. Parasym- pathetic nerves are derived from the vagus. Referred pain of appendix is felt at umbilicus, similar to that of small intestine and testis.
Lymphatic Drainage
Most of the lymphatics pass directly to the ileocolic nodes, but a few of them pass indirectly through the appendicular nodes situated in the mesoappendix.
HISTOLOGY
The lumen of appendix is very narrow. There are no villi. The epithelium invaginates to form crypts of Lieberkühn. Muscularis mucosae is ill defined. Submucosa reveals many lymphoid masses. That is why it is called the abdominal tonsil. Muscularis externa comprises two layers. Outermost is the serous layer.
ASCENDING COLON
Ascending colon is about 12.5 cm long and extends from the caecum to the inferior surface of the right lobe of the liver. Here it bends to the left to form the right colic flexure. It is covered by peritoneum on three sides.
Anteriorly, it is related to the coils of small intestine, the right edge of the greater omentum, and the anterior abdominal wall. Posteriorly, it is related to the iliacus, the quadratus lumborum, the transversus abdominis, the lateral cutaneous, ilioinguinal, and iliohypogastric nerves and the right kidney.
RIGHT COLIC FLEXURE (HEPATIC FLEXURE)
Right colic flexure lies at the junction of the ascending colon and transverse colon. Here the colon bends forwards, downwards and to the left. The flexure lies on the lower part of right kidney. Anterosuperiorly, it is related to the colic impression on inferior surface of the right lobe of liver.
TRANSVERSE COLON
 |
| Relation of transverse mesocolon to anterior border of pancreas |
Transverse colon is about 50 cm long and extend across the abdomen from the right colic flexure to the left colic flexure. Actually, it is not transverse, but hangs low as a loop to a variable extent. It is suspended by the transverse mesocolon attached to the anterior border of pancreas, and has a wide range of mobility.
Anteriorly, it is related to the greater omentum and to the anterior abdominal wall. Posteriorly, it is related to the second part of the duodenum, the head of the pancreas, and to coils of small intestine.
LEFT COLIC FLEXURE (SPLENIC FLEXURE)
Left colic flexure lies at the junction of the transverse colon and the descending colon. Here the colon bends downwards, and backwards. The flexure lies on the lower part of the left kidney and diaphragm, behind the stomach, and below the anterior end of the spleen. The flexure is attached to the eleventh rib (in the midaxillary line) by a horizontal fold of peritoneum, called the phrenicocolic ligament. This ligament supports the spleen and forms a partial upper limit of the left paracolic gutter.
DESCENDING COLON
Descending colon is about 25 cm long and extends from the left colic flexure to the sigmoid colon. It runs vertically up to the iliac crest, and then inclines medially on the iliacus and psoas major to reach the pelvic brim, where it is continuous with the sigmoid colon. The descending colon is narrower than the ascending colon.
Anteriorly, it is related to the coils of small intestine.
Posteriorly, it is related to the transversus abdominis, the quadratus lumborum, the iliacus and the iliohypogastric, ilioinguinal, lateral cutaneous, femoral and genitofemoral nerves; the gonadal and external iliac vessels. psoas muscles;
SIGMOID COLON (PELVIC COLON)
Sigmoid colon is about 37.5 cm long, and extends from the pelvic brim to the third piece of the sacrum, where it becomes the rectum. It forms a sinuous loop, and hangs down in pelvis over the bladder and uterus. Occasionally, it is very short, and takes a straight course. It is suspended by the sigmoid mesocolon and is covered by coils of small intestine.
SOURCE BD CHAURASIA'S Anatomy
Comments
Post a Comment